Skin care
- Baby's skin is delicate and is susceptible to becoming dry and broken. It needs gentle care.
- Use fragrance- free bathing gel or just water for a baby's bath.
- The skin of your baby may look dry and will peel off before one month old. This is perfectly normal and you don't need to put body lotion on your baby.
- When your baby is already one month old, you may apply a mild body lotion on your baby after bath to prevent loss of moisture in dry weather.
- Avoid exposing baby under the sun directly when going out. Use an umbrella or put a bonnet on your baby to protect him from the sun. Do not apply sunscreen on your baby to avoid causing skin irritation or allergy.

Common skin problems among babies

Milia
Descriptions
Cause
- Related to the premature development of the skin glands
Symptoms
- Common among newborns
- Appear as white or yellow dots of the size of a needle tip, flat on touching
Affected areas
- On forehead, cheeks, chins and nose
- Appears as white bumps on some babies' gum (Epstein's pearls)
Treatment and prevention
- Usually disappear on their own 2-3 weeks after birth. No specific treatment is needed.
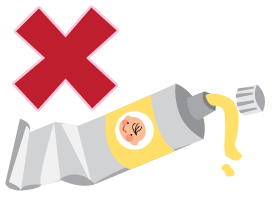
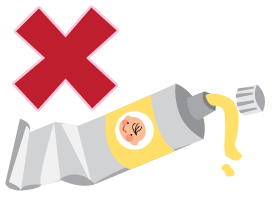
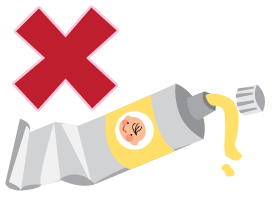
- Do not squeeze or apply medications

Neonatal Acnes
Descriptions
Cause
- Due to mother's hormones crossing the placenta to the baby during pregnancy
Symptoms
- Small raised reddish bumps
- Commonly found a few days or weeks after birth
Affected areas
- On foreheads and cheeks
Treatment and prevention
- Shall disappear on their own within 3 months after birth. No special treatment is needed.
- Keep skin clean and dry. Do not squeeze or apply any medications

Erythema Toxicum
Descriptions
Cause
- Unknown
Symptoms
- White or yellow dots of the size of a needle tip, surrounded by blotchy redness
- Commonly appear 2-3 days after birth.
Affected areas
- Commonly found on cheeks, trunk, back, hands and feet
Treatment and prevention
- Usually disappear on their own within a few days to weeks after birth. No special treatment is needed.
- Do not squeeze or apply medications

Seborrhoeic Dermatitis (Commonly known as ‘cradle cap')
Descriptions
Cause
- Not completely clear
Symptoms
- Common among newborns
- Appears slightly red
- Small oily flakes or yellowish thick scales adhering to the scalp or eyebrows, forming a layer of scab
- Commonly found when baby is 3 weeks to 3 months old
- Subsides gradually at around 6 months old
Affected areas
- Areas with lots of skin glands
- e.g. head, forehead, cheeks, eyebrows, ears, armpits, belly and the folds between the thighs
Treatment and prevention
- Keep baby's skin clean.
- Rinse the affected areas with water. Do not use soap / bath gel.
- Apply moisturizing cream after cleaning to keep the skin moist
- For thick scales on scalp, apply olive oil and leave on the scalp for 20 minutes to soften them. Wipe the scales off gently with cotton swabs.
- Rinse with baby shampoo. Use a comb to clear away the adhered patches


Infantile Eczema/Atopic Dermatitis
Descriptions
Cause
- Unknown
- Not infectious
- More likely to appear in babies with family members suffering from allergies (e.g. asthma, allergic rhinitis) or being allergic to certain substances (e.g. pollen, detergents, dust or foods)
Symptoms
- Commonly found in babies 2-3 months old
- Appears red and dry. Sometimes, small blisters appear and scabs are formed when blisters broken
- Baby will scratch the affected areas due to itchiness
- Skin becomes thick and hard after scratching
- In most cases, it appears before the age of 5 and fades away after 15. Some may persist into adulthood
Affected areas
- Cheeks, elbows, knees, trunk and folds between thighs.
- The affected areas will vary with age.
- Commonly found on neck and folds on limbs when reach the age of 2.
Treatment and prevention
- Keep skin clean and moist
- Bathe baby with lukewarm water and non-alkaline bathing gel
- Pay attention to cleaning the skin folds
- Apply fragrance-free moisturizer after bath
- Trim baby's nails regularly to reduce the chance of skin injury by scratching. May put cotton gloves on baby if the baby scratches a lot
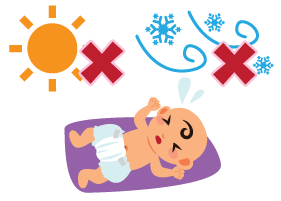
-
Pay attention to the temperature and humidity of the environment. Avoid exposing directly to strong sunlight or cold wind.
-
Clean your home with wet cloth or vacuum cleaner to remove dust
- Do not keep furry pets
-
Choose cotton clothes for your baby. Avoid clothes made of wool, nylon or silk to be in direct contact with baby's skin.

- Use mild detergent to wash baby's clothes. Rinse with water thoroughly.
- Breastfeeding may prevent eczema.
- If symptoms persist or get worse, consult your doctor before applying any medications.

Heat Rash/Prickly Heat
Descriptions
Cause
- Usually in hot weather
- Occurs when wrapped in excessive clothing
- Caused by sweat staying on skin
Symptoms
- Small raised red spots
Affected areas
- Neck, back and chest
Treatment and prevention
- Clean with a towel and water
- Dress in appropriate amount of clothing
- Keep skin dry and cool; reduce sweating
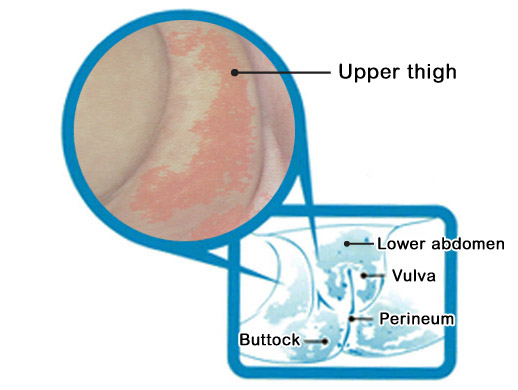
Diaper Rash/Nappy Rash
Descriptions
Cause
- When skin is irritated by urine and faeces
Symptoms
- Begins as red spot, then develops into small raised reddish rash
- Sometimes spread to all areas covered by diaper
Affected areas
- Vulva, perineum, buttocks and areas wrapped by diapers.
- Sometimes may appear on lower abdomen and upper part of the thighs.
Treatment and prevention
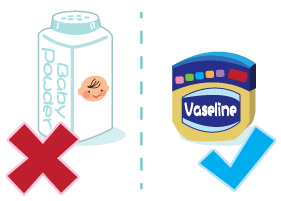
- Keep baby's bottom clean and dry.
- Clean with damp cotton wool when changing diapers.
- Allow the bottom to air dry. Apply a thin layer of oil-based moisturizer (Vaseline) or zinc oxide cream to keep the urine and faeces from direct contact with the skin.
- Do not use talcum powder. It will mix with urine or sweat to clog the sweat pores and worsen the condition.
*If the above symptoms persist, please consult your doctor.
Breastmilk or infant formula?
Children's early nutrition and dietary patterns have tremendous impact on their future growth and health. Therefore, how you are going to feed your baby is an important decision.
Breastfeeding is the natural and superior way of feeding. Breastmilk can provide babies with all the necessary nutrients as well as natural antibodies. The composition and supply of breastmilk will self-regulate with the baby's growing needs. The intimate physical contact during breastfeeding enhances the bonding between mother and baby, thus brings satisfaction to the mother. These unique properties of breastfeeding cannot be replaced by infant formula feeding.

Some mothers are unable to breastfeed or they may prefer infant formula for some reasons. Infant formulae can provide the basic nutrients for babies. However, parents must pay attention to the proper preparation of infant formula and ways of bottle feeding.
Spitting up
Babies may cry a lot or suck too rapidly in feeding. This will result in air being swallowed and gathered in the stomach. They may spit up a little milk together with the air during burping or when being laid down after feeding. Clean your baby well with a towel after spitting to decrease the chance of having rash caused by skin irritation.
Tips to reduce spitting up
- Feed baby in a calm mood and peaceful surroundings.
- Do not interrupt or distract your baby during feeding.
- Don't wait till your baby is too hungry to feed to avoid him suckling/ sucking too rapidly.
- Avoid over-feeding your baby. Feed on demand no matter you are breastfeeding or use bottle feeding.
- Make sure your baby suckles properly when breastfeeding.
- Hold your baby in your arm instead of letting him lie down when bottle-feeding.
- Hold your baby close in a semi-upright position with his head and neck resting on your elbow so he can breathe and swallow comfortably.
- Hold the bottle horizontally or slightly tipped when bottle feeding, to prevent the milk from pouring too quick. This allows your baby to control the milk flow through active sucking, and can also avoid over-feeding him.
- Burp your baby half way during feeding or when baby has finished suckling one of your breasts.
- Burp your baby until he has burped. However, babies do not burp all the time. In that case, you can continue to feed your baby after a few minutes of burping.
- Hold your baby upright for about 10-20 minutes after burping before putting him down. Don't put a pillow directly under your baby's head to avoid the risk of suffocation.


The difference between spitting up and vomiting
Spitting up:
Vomiting:

Burping
- Burp your baby after feeding or half way through feeding can reduce spitting up.
- Although breastfed babies are less likely to spit up than bottle-fed babies, they still need to be burped.
- Skills in burping video
How to burping your baby
Heading: How Should Babies be Burped?
Super: I've Got Hiccups!
Narrator: How should babies be burped?
Before burping, place a cloth on your shoulder and hold your babies upright with their chin resting on your shoulder.
Super: Rest Babies' Chin on your Shoulder
Narrator: Gently pat or rub their back for a few minutes.
Super: Gently Pat or Rub Babies' Back
Narrator: You can also sit them on your lap.
Super: Sit Babies on your Lap
Narrator: Place the palm of your hand flat against their chest and support their chin and jaw.
Super: Support Babies' Chest, Chin and Jaw
Narrator: Lean them slightly forwards
Super: Lean Babies forwards Slightly
Narrator: and gently rub or pat their back with your spare hand for a few minutes.
Super: Gently Pat or Rub Babies' Back
Narrator: To prevent food from being spat out, keep them upright for 10 to 20 minutes after burping.
Super: Family Health Service
Department of Health
www.fhs.gov.hk
June 2024
Narrator: This video is produced by the Family Health Service of the Department of Health.
Hiccups
- Hiccups are caused by sudden involuntary contractions of baby's diaphragm
- It is normal for babies to hiccup after feeding and they are not actually bothered
- Most hiccups have no obvious reasons
- Babies could have short period of hiccups when they have a full stomach after rapid sucking. Hiccups will stop without any treatment.
- If you do want to do something to reduce the hiccups, you may let your baby suckle again on your breast. You can give your baby some lukewarm water if he is bottle-fed. Burping may be another way you can do.
Learning how to sleep
The advantages of having regular routines
When babies start to get used to their surroundings, parents should start establishing regular daily routines for them. Having regular feeding, bathing and sleeping hours can make the environment predictable and add a sense of security to your baby. By having a stable environment, your baby will be less likely to develop behavioural and emotional problems. You will then be easier to understand her temperament.

Characteristics of babies' sleep

While the “job” of babies is eating and sleeping, you need to learn more about the characteristics of your baby's sleep and establish a regular sleep routine for her.
Just as inside the mother's womb, babies sleep whenever they are tired without taking note of day or night in their first couple of months. They have short sleep periods of 3 to 5 hours. They also wake up easily as about half of their sleep time is in the light sleep state.
When they are 3 months old, they can sleep for longer hours. Two-third of their sleep takes place at night time. When they reach 6 months old, around 50% of the babies can sleep at night for 6 hours.
Sleeping hours
The sleeping hours will change as our child grows:
| Age | Total sleeping hours in 24-hour period* (include both day and night sleep) |
|---|---|
| 0-3 months old | ~ 14-17 hours |
| 4-11 months old | ~ 12-16 hours |
*Reference: WHO guidelines on physical activity, sedentary behaviour and sleep for children under 5 years of age. Geneva: World Health Organization; 2019. Licence: CC BY-NC-SA 3.0 IGO.
The ideal and safe sleep environment
Room temperature and ventilation
- Room temperature should be comfortable and ventilation good.
- Do not put on too much clothing or blankets on the baby to avoid her being too warm and unable to sleep.
- Check the baby's nape of her neck. Feeling just warm means that your baby is comfortable. If there is sweat, it may mean that it is too warm for your baby.
Sounds
Some babies prefer a quieter environment to sleep. Yet, some babies fall asleep easier with some sounds, so playing soft music and humming lullabies may help. Caregivers may facilitate their babies' sleep by arranging a suitable environment which fits the babies' temperamental characteristics and sleep patterns and behaviours.
Beddings
- Your Baby does not need pillow to sleep. Don't put soft objects and loose bedding at where your baby sleeps to protect her from suffocation. These include diapers, fluffy blankets or duvets, pillow-like bumpers, stuffed toys, etc.
- Cotton bed sheets and blankets are the best for the baby as they reduce the chance of getting allergies
- When using a blanket, be careful not to cover your baby too loosely. To avoid suffocation, tuck the edges of the quilt under the firm mattress, or use sleeping bag / wearable blanket for baby. Do not cover her head and keep her hands out of the blanket to avoid suffocation.
- Some caregivers swaddle their baby at bedtime to help her feel secure. However, swaddling too tightly may restrict her leg movement and affect the normal development of hip joint. Besides, make sure the baby's head and face are not covered to avoid affecting breathing and body heat dissipation. Similarly, if swaddling too loosely which may increase the risk of having the baby's airway being obstructed and her body being strangulated. Let your baby sleep in supine position when swaddled. In general, to avoid any accident, swaddling is not recommended for a baby around 2 months old or when she starts trying to roll over.
Learning how to sleep
Differentiating day and night
Babies cannot tell day from night. How to teach babies to stay active during daytime and go to sleep at night seems to be a big challenge for parents. Parents however can start by emphasizing the difference in light and introducing a regular schedule to enable babies to establish their daily routines.
Light
- There should be difference in the room light. The room should be well-lit in the daytime while lighting should be dimmed when it is time to sleep at night.
- Some babies may wake up crying for scaring of the darkness. You may switch on a night-light to reassure your baby.
Regular daily routines

- When your baby is awake in the daytime, you may play and talk actively with her to prevent your baby from sleeping too much during the day. When your baby gets tired as shown by having drooping eyelids, rubbing her face against you or yawning, let your baby have some sleep. On the other hand, you have to minimize her activities at night.
- Try to finish the house chores as soon as possible, feed your baby and let her settle down. You can hum a tune and talk to your baby to calm her down. Then put your baby in bed, let your baby fall asleep on her own.

Establishing bedtime routine
Developing regular sleep routine – English
Scene: Daddy plays with baby.
Mother: Baby, It's time to sleep.
Daddy: Oh, she is tired now. Let her sleep in my arms.
Mother: It's not a good idea. Baby will only sleep when you hold her. Actually, I have already helped her develop a regular sleep routine.
Daddy: Regular sleep routine?
Narrator: When your baby reaches 2 to 3 months old, you can help her develop a regular sleep routine. This is about associating your baby's particular daily activities with going to sleep. In this way, babies learn to fall asleep on their own after the series of activities. Babies have different characteristics. You can help your baby develop sleep routines according to her characteristics and habits. Here are two examples.
Sub-heading: Feed your baby. Burp her and hum a tune to her. When your baby gets sleepy, put her in bed. Turn off the light.
Narrator: Here is another example.
Sub-heading: Bathe your baby. Feed your baby. Burp her. Have a little chat with your baby. Put your baby in bed when she gets sleepy. Play soft music and dim the light. Let her fall asleep on her own. Developing regular sleep routine for your baby makes baby care easier for you.
- When babies reach 2 to 3 months old, parents can try to set up a regular bedtime routine for them, i.e., helping babies to learn to associate particular activities with going to sleep and let them fall asleep on their own.
- When babies have got used to fall asleep in their bed, it is easier for them to fall back to sleep even if they wake up in the middle of the night.
- You can set up a special bedtime routine for your baby according to her temperament and daily routines.
Poor Sleeping Habits
Never let your baby develop poor sleeping habits. For instance, some babies can only fall asleep when being taken in their parents' bed or arms, being rocked or fed. Once if these undesirable patterns have developed into routines in your baby, it means that your baby would depend totally on your attention and company to fall asleep every night; moreover, your baby could hardly fall back to sleep without your warm embrace or comfort derived from suckling/sucking on the teat.
What happen if your baby falls asleep during feeding?
- It is common for babies to fall asleep during feeding, especially those under 1 month old who need to be fed frequently.
- If your baby falls asleep during feeding, you can stop feeding her. Burp your baby and put her on bed. You can feed her a bit earlier next time so that your baby won't be too tired at feeding time.

- As your baby needs less frequent night feeding when she grows, it would be a good time for you to establish sleep routine for your baby to help your baby sleep on her own.
- If your baby wakes up and cries at night, you need to find out what she needs such as changing a wet nappy, company or feeding. You should not feed your baby if she is not hungry to avoid your baby depending on sucking or suckling to fall back to sleep.
Note: Establishing a successful sleep routine for your baby includes steps of having the baby fed, nappy changed and your baby starts to show signs of tiredness before you put her in bed. There is no quick fix to baby's sleeping problems.
Therefore, in developing a sleep routine for your baby, you need to be patient and persistent and pay attention to factors that may affect your baby's sleep.
Baby's safe sleeping position and environment
Baby's safe sleeping position and environment
Narrator: Let babies sleep on their backs
Sleep in their own cot
Dress them in light and comfortable wear
They do not need pillows
Leave their arms uncovered
Don't place any soft and fluffy objects in the cot
Leave no gaps between the mattress and the cot
Distance between the vertical bars of the cot should be less than 6 cm
Place the baby cot next to the parents' bed
If you need to share a bed with your baby for some reason, give him a separate blanket; for a baby aged less than 3 months old, you may place him in a basket
Don't take alcohol or drugs if you are to sleep with babies.
Keep good ventilation and a comfortable temperature. There should not be any smokers in the family
Don't leave babies alone on a bed or sofa without guards
Lastly, breastfeeding can protect against SIDS (sudden infant death syndrome in subtitle), after feeding and burping the babies, put them in the cot when they look sleepy. That helps them build a good sleeping habit.
Please visit www.fhs.gov.hk
Preventing Sudden Infant Death Syndrome (SIDS)
SIDS or cot death refers to sudden death of a baby while sleeping during the first year, most commonly around 1-4 months old, with an unknown cause. You can prevent it by using preventive practices mentioned above. Sleeping on the back gives your baby the best protection from SIDS.
In addition, a smoke-free environment, vaccinations and breastfeeding can also reduce the risk in your baby.

How to create a safe sleep environment?
Ensuring the safety of your baby's sleep environment is of paramount importance. An unsafe sleep environment can be fatal to your baby.
Here is a checklist of a safe sleep environment for babies. How many of these are you doing?
-
Sleeping with your baby in the same room in separate beds

-
The distance between the bars of the crib should be less than 6cm (2.5″)
-
Remember to pull up and lock the rail of the crib when you leave your baby alone in crib

-
The size of the mattress should be fitted in the crib to prevent baby from rolling into the gap
-
Make sure baby's face and head are exposed above the blanket to prevent smothering and overheating
-
Let your baby wear light and comfortable clothing at bedtime
-
Keep the room well-ventilated with comfortable temperature for your baby
The following 4 situations may threaten your baby's sleep safety. ‘Watch out' and ‘Don't do' these:
-
Mattress too soft and thick will make baby easily roll over to a face- down position which may lead to suffocation.
-
Use baby pillow or let baby sleep on big, soft and fluffy beddings or other objects. These include light, soft blankets or duvets, sheep skin, bean bag chair, bumper, pillows or stuffed toys. Your baby could be smothered easily when the objects cover the baby.
-
Place things other than beddings (e.g. toys and clothing) in baby's bed.
-
Too much clothing or too many blankets can make the baby too hot.
Safety notes on using a baby carrier
Many parents like carrying babies in a baby carrier for the convenience of care and the ease of going about. Baby carriers can be found in different styles. They can basically be divided into the carrier and sling types; or the soft and the structured/backpack types. Different style has its advantages and disadvantages. Whatever type you use, you must pay attention to the safety issues in using baby carriers. Put your baby in carrier no more than 1 hour each time.
Sling type

Wrap-around sling

Ring sling

Pouch sling
Carrier type

Mei tai

Traditional mei tai

Traditional mei tai
Backpack

Soft structured carrier
Can babies skip vaccination?
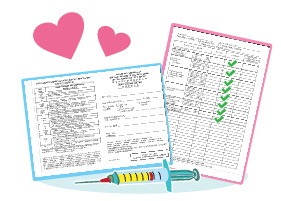
You can bring your newborn to 5 year old child to the Maternal and Child Health Centres of Department of Health(DH), private hospitals or clinics for immunisation. The School Immunisation team of DH will visit primary schools to provide injection to students. You can also bring your child to private doctors for vaccination.
Vaccinations provided in Maternal and Child Health Centres (DH) for 1-4 months olds
Besides those vaccines recommended by the Department of Health for inclusion in the Hong Kong Childhood Immunisation Programme, some private doctors and hospitals may provide other vaccines to protect children from certain infectious diseases. Parents should seek advice from their family doctor before getting their children immunised.
What to do when your baby has fever?
Many parents are worried about what may come if their babies have got fever. Fever simply means a higher than normal body temperature, and is something that is experienced by every child one time or another. It is important to learn about the causes for fever and how to care about babies with fever and to watch out for signs of deterioration of the condition.
The normal temperature of a child varies depending from which part of the body temperature is taken:
| Method used | Children's normal body temperature |
|---|---|
| Infrared Tympanic (eardrum) | 35.8°C – 38°C (96.4°F – 100.4°F) |
| Digital Axilliary (armpit) | 34.7°C – 37.3°C (94.5°F – 99.1°F) |
| Digital Rectal | 36.6°C – 38°C (97.9°F – 100.4°F) |
Q: Why would children get fever?
Fever is a symptom of possible underlying illnesses. Fever is also a physiological response to vaccination. It is a sign that the body's immune system is functioning normally against infections. If your baby has fever after vaccination, he will be likely to recover within 2 to 3 days. All you need is simply to take good care of the child and monitor his body temperature.

Q: Should I bring my baby to the doctor immediately whenever she has a fever?
If your baby develops a fever after vaccination, you can take care of her according to the advice given by the health personnel first. However, if it is not related to the vaccination, she could be ill. You should bring her to the doctor immediately. Although fever does not usually indicate serious underlying illness, however, if your baby is 2 months old or younger, has problem in immune system, or has other special health problems, you should take her to the doctor immediately even though her body temperature is at the upper limit of the normal range.
How to measure a child's temperature?
Apart from complying with the doctor's treatment and prescription, you should closely monitor the conditions of your baby and give proper care at home. You may check your baby's body temperature every 4 hours if necessary to monitor the fever.
Common types of thermometers for young children
| Types of Thermometers | Digital | Infrared Tympanic |
|---|---|---|
| Body parts to be checked | Armpit and Rectum | Eardrum |
| Accuracy |
|
The sensor should be placed correctly. |
| Price | Economical | More expensive |
| Convenience | Easy to use |
|
| Remarks | Oral temperature taking is not recommended for babies and young children Armpit temperature taking is the safest and may be preferred for babies under 3 months. Some may consider the rectal route as unacceptable and has risk of injury to the bowel. |
Not suitable if
|
Note: Do not use mercury thermometer for safety reason as it may break easily and has toxic mercury spillage as a result.
Digital Thermometer
Things needed when using the digital thermometer:
- Digital thermometer
- 70% alcohol
- Cotton wool balls
- Lubricant (for rectal use)
- Watch / Timer
- Diapers (when necessary)
Steps in using a digital thermometer
For a better understanding on the use of digital thermometers, you can watch the demonstration video
Steps in using Digital Thermometer
Narrator: Digital thermometers are used to test baby's rectal and axillary temperature, Sterilize the thermometer with alcohol before use, then switch it on.
Sub-Heading: Taking the axillary temperature
Narrator: Hold the baby in your arm or lay her on the bed. Put the end of the thermometer in firm and direct contact with her armpit. Hold the thermometer in place by pressing baby's arm against her body. Keep the thermometer in place until you hear the beeps.
Sub-Heading: Taking the rectal temperature
Narrator: Taking rectal temperature is similar to taking axillary temperature. Sterilize the thermometer first and apply some lubricant over the sensor end. For newborns and young infants, lay them on the bed when taking rectal temperature. Lift up the baby's feet and seperate her buttocks. Insert the thermometer into her anus to about 1.3 to 2.5cm, that is, about half to full length of your finger tip. Hold it in place and avoid pushing it in too far. Clean the baby's anus and place her in a safe place before you read the temperature. Record the temperature reading and turn off the thermometer. Clean the thermometer with alcohol before storing it.
Infrared Tympanic Thermometer
Notes on using the infrared tympanic thermometer
- As there is temperature difference between ears, always take temperature from the same ear during the period of temperature monitoring.
- Take 3 measurements from the same ear at a time and settle on the highest temperature.
- Refer to the manufacturer's instructions for the normal temperature range.
Steps in using infrared tympanic thermometer
For a better understanding on the use of the infrared tympanic thermometer, watch the demonstration video.
Steps in using infrared tympanic thermometer
Narrator: Before using the tympanic thermometer, calibrate it according to the manufacturer's instruction regularly. Use a new probe cover on the thermometer every time. Straighten the baby's ear canal to detect the temperature accurately. For babies under one year old, pull their ears straight back. For children over one year old and adults, pull their ears backward and upward. Every time, take 3 measurements for the same ear and take the highest reading as the baby's temperature. Always refer to the manufacturer's instruction for the reference normal temperature range, as it varies with different brands and models. Clean the probe according to the instruction every time after use. Discard the probe cover after use.
Caring for your feverish baby at home
| Method | Applicable conditions | DOs | DON'Ts |
|---|---|---|---|
Taking prescribed medication |
|
|
Give the baby medication in whatever ways and at whatever time you like because overdose can be harmful to your baby |
Dressing your baby comfortably |
Anytime |
|
Put on too many layers of clothes will overheat the baby. |
Keeping good ventilation |
Anytime |
Keep the room ventilated by having the windows opened or turning on an air-conditioner or electric fan. |
Shut all windows and door |
Extra fluid intake |
Anytime |
|
No extra fluid intake apart from the daily milk intake |
Having enough rest and nutrients |
Anytime |
|
|
Sponging with lukewarm water |
To make your baby feel more comfortable when she:
|
|
Avoid using cold water and alcohol to cool down the fever, as it could cause shiver and the body temperature could rise instead. |
Signs to seek further medical advice:

- You can use the above methods together to reach the optimal results. However, pay close attention to your babies' conditions when applying these methods.
- Whatever the reason for your baby's fever, if any one of the following signs appears in the baby or you are concerned/distress, you should take him to the doctor immediately:
- Having a fit
- Developing rash
- Being less well or not feeding well
- Having persistent fever
- Having signs of dehydration
- Taking care of a baby with fever and monitoring his situation day and night can be demanding and exhausting. You can consult experienced relatives or friends in managing your baby's fever. Always seek support from and share your stress with your family.

